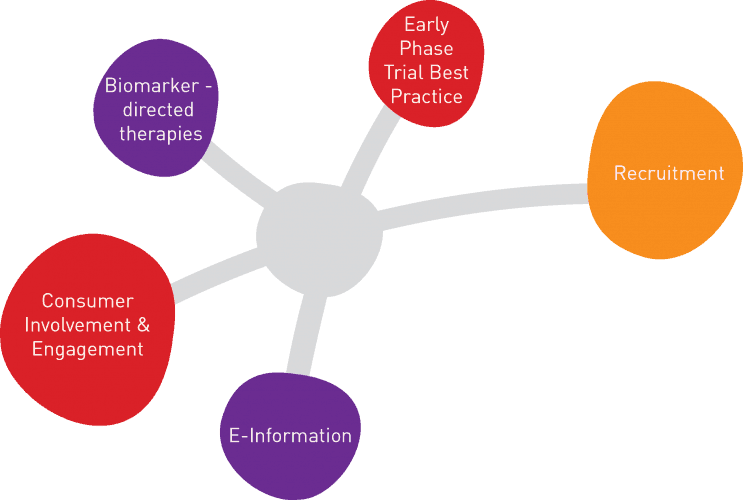
CT:IQ Overview
In 2018 Bellberry Ltd, ACTA, NHMRC Clinical Trials Centre and The George Institute have formed a consortium called Clinical Trials: Impact & Quality (CT:IQ). CT:IQ’s mission is to develop and implement recommendations that will improve the impact, quality and efficiency of clinical trials, leading to more rapid, lower cost and higher quality evaluation of healthcare interventions in Australia.
CT:IQ acts as a platform for all stakeholder voices to come together. By forming project teams to identify challenges, they aim to explore, solve and implement solutions in both investigator-led and industry trials sectors. This will lead to a more meaningful integration of clinical trials into the Australian health system, resulting in better healthcare and better outcomes for patients, participants and the community as a whole. To participate or for more information visit www.ctiq.com.au or email info@ctiq.com.au
Project 1: Consumer Involvement & Engagement (CI&E) Toolkit
CI&E is critical to fostering consumer access to innovative therapeutic solutions and delivering better health outcomes for patients, participants and the community. This collaborative project between CT:IQ and the Australian Clinical Trial Alliance (ACTA) will foster best practice across the research sector by providing a mechanism to share resources both locally and internationally via a public website. This platform will provide tools to support CI and CE within Clinical Trials (CTs) activities and seek opportunities to increase the awareness, knowledge and capacity of the wider community. The content specialist, Tanya Symons was appointed in April, along with platform developer, Orchard. The first workshop socialising some of the tools was held on 6 May. The website will be launched in Quarter 4.
Project 2: eConsent adoption: Barriers and Recommendations
eInformation and eConsent improve the quality of the consenting experience, increases patient engagement as well as the accessibility and opportunity for participation, however currently there is limited uptake in both the investigator-initiated and industry-led CT sector in Australia and globally. This project aims to understand the barriers to eConsent adoption in Australia and to produce practical recommendations and actions to increase uptake of e-information. The results will be released at the CT:IQ Steering Committee Meeting 24-June!
Project 3: Early Phase Trials Best Practise
There is currently no single source of best practice outlining expectations for the conduct of early phase, and crucially Phase I Clinical Trials in Australia. This project aims to identify, summarise and test recommendations for best practise conduct of early Phase Clinical Trials. This project utilises the wealth expertise and experience from the CT:IQ Steering and Executive Committees including NSW Health, Linear, CMAX, Macquarie University, Biotronik Orygen, Centre for Biostatistics and Clinical Trials at the Peter MacCallum, Cancer Trials Australia, Icon Cancer Group, a consumer representative, VCCC, the Medical Technology Association of Australia and Bellberry Ltd. The project is in the evidence-gathering phase. The guidance will be released in December 2019.
Project 4: CT Recruitment: Barriers and Recommendations
This project is focused on addressing sub-optimal rates of Clinical Trial participation and will provide practical guidance for sites for optimising recruitment which is broadly applicable and translational. Similar to Project 3, this project is also in the evidence gathering phase with a survey on the barriers and enablers for Clinical Trial recruitment launching within the month so please keep an eye out!
Project 5: Guidelines for biomarker-directed therapies in personalised medicine: Tools for assessment
Currently, there is a lack of guidance around the criteria that should be used to assess evidence for individualised/personalised clinical decisions especially linked to patient’s biomarker profile. This collaborative project between CT:IQ, the NHMRC Clinical Trials Centre (CTC) and Utrecht University will develop a theoretical framework which will be valuable for policy makers including the PBAC and MSAC as well as clinicians to optimise patient treatment decisions. This project is just launching now.